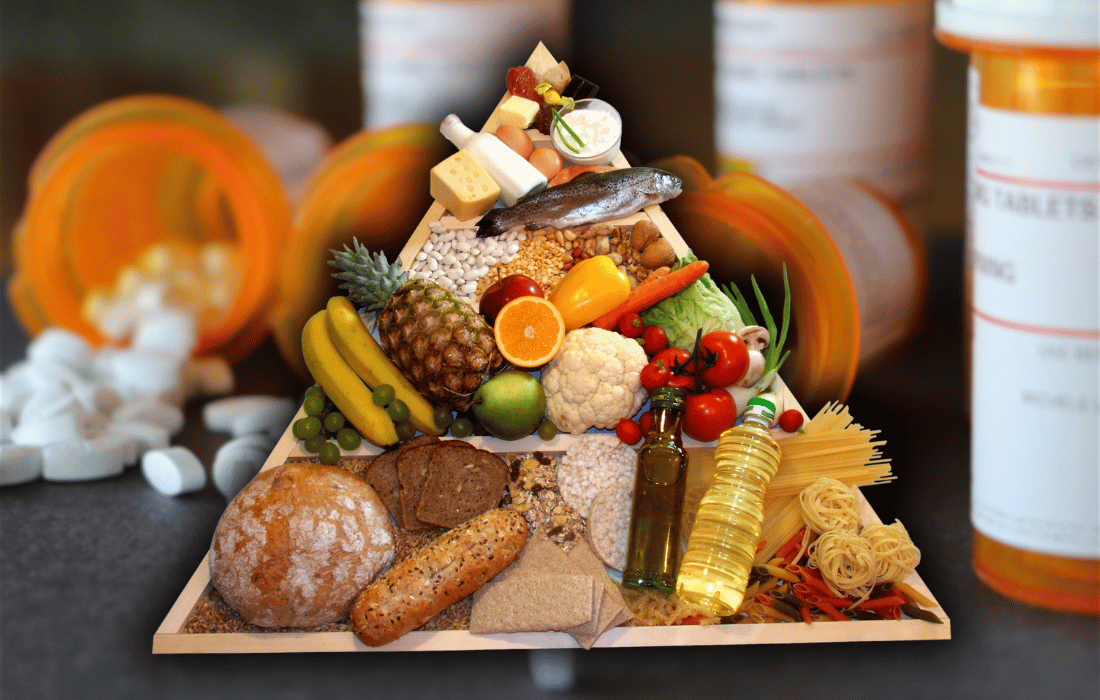
The origins of the U.S. Dietary Guidelines date back to 1977, when the Senate Select Committee on Nutrition and Human Needs published its “Dietary Goals for the United States.” This initiative laid the groundwork for what would become the USDA’s official Dietary Guidelines for Americans. The objective was simple: to help citizens make informed dietary decisions in the interest of public health. Unfortunately, as with many well-intentioned policies, the guidelines were quickly entangled in politics, flawed science, and powerful food industry lobbying.
Initially, the guidelines promoted low-fat, high-carbohydrate diets, elevating refined grains and vegetable oils while demonizing saturated fats and red meat. Science journalist and nutrition researcher Nina Teicholz, author of “The Big Fat Surprise,” has thoroughly documented how these assumptions were not only unsupported by strong scientific evidence but have been proven actively harmful by modern research. Her critique of the 2025 U.S. Dietary Guidelines highlights that they continue to perpetuate outdated recommendations rooted more in politics than evidence-based nutrition.
Why the Current U.S. Dietary Guidelines Remain Nutritionally Flawed
Despite mounting scientific evidence, the U.S. Dietary Guidelines continue to recommend outdated nutritional advice that contributes to rising rates of obesity, diabetes, and metabolic disorders. This section examines two of the most harmful recommendations that remain entrenched in the national nutrition policy.
The Continued Vilification of Saturated Fat
Despite robust scientific evidence debunking the hypothesis that saturated fat causes cardiovascular disease, the current guidelines still recommend limiting saturated fat intake to less than 10% of total daily calories. This is in direct contradiction to findings from meta-analyses of randomized controlled trials and large cohort studies, such as the PURE study, which demonstrated no consistent association between saturated fat intake and increased cardiovascular risk.
Low-carbohydrate, high-fat dietary patterns have repeatedly been shown to:
Enhance insulin sensitivity
Promote sustainable weight loss
Improve lipid profiles (higher HDL, lower triglycerides)
Reduce inflammatory markers
Yet the guidelines remain entrenched in a fat-phobic narrative that benefits food manufacturers selling low-fat, ultra-processed substitutes laden with sugar and synthetic ingredients.
High-Carbohydrate Diet Recommendations Contribute to Metabolic Dysfunction
The USDA recommends that 45–65% of daily calories come from carbohydrates. This recommendation assumes that all carbohydrates are metabolically benign, overlooking the critical distinctions between refined grains, whole grains, and fiber-rich vegetables.
Numerous studies have linked high carbohydrate intake, particularly from refined and processed sources, to:
Type 2 diabetes
Non-alcoholic fatty liver disease (NAFLD)
Increased triglyceride levels and decreased HDL cholesterol
These conditions are now endemic in the American population. Continuing to recommend high-carb diets in the face of an obesity and diabetes epidemic is not just outdated — it’s irresponsible.
Conflicts of Interest Within the Dietary Guidelines Advisory Committee (DGAC)
The USDA is uniquely positioned to promote both agricultural interests and public health, creating an inherent conflict of interest. It is tasked with supporting commodity agriculture (corn, wheat, soy) while simultaneously issuing dietary recommendations that are supposed to prioritize health. Unsurprisingly, the guidelines are heavily skewed toward promoting the consumption of subsidized crops.
Many members of the Dietary Guidelines Advisory Committee have documented financial ties to organizations such as:
The National Dairy Council
The International Life Sciences Institute (ILSI)
The American Beverage Association
These conflicts raise legitimate concerns about the objectivity and credibility of the guidelines. Recommendations are often based on weak observational studies, while high-quality intervention studies that contradict the narrative are ignored or minimized.
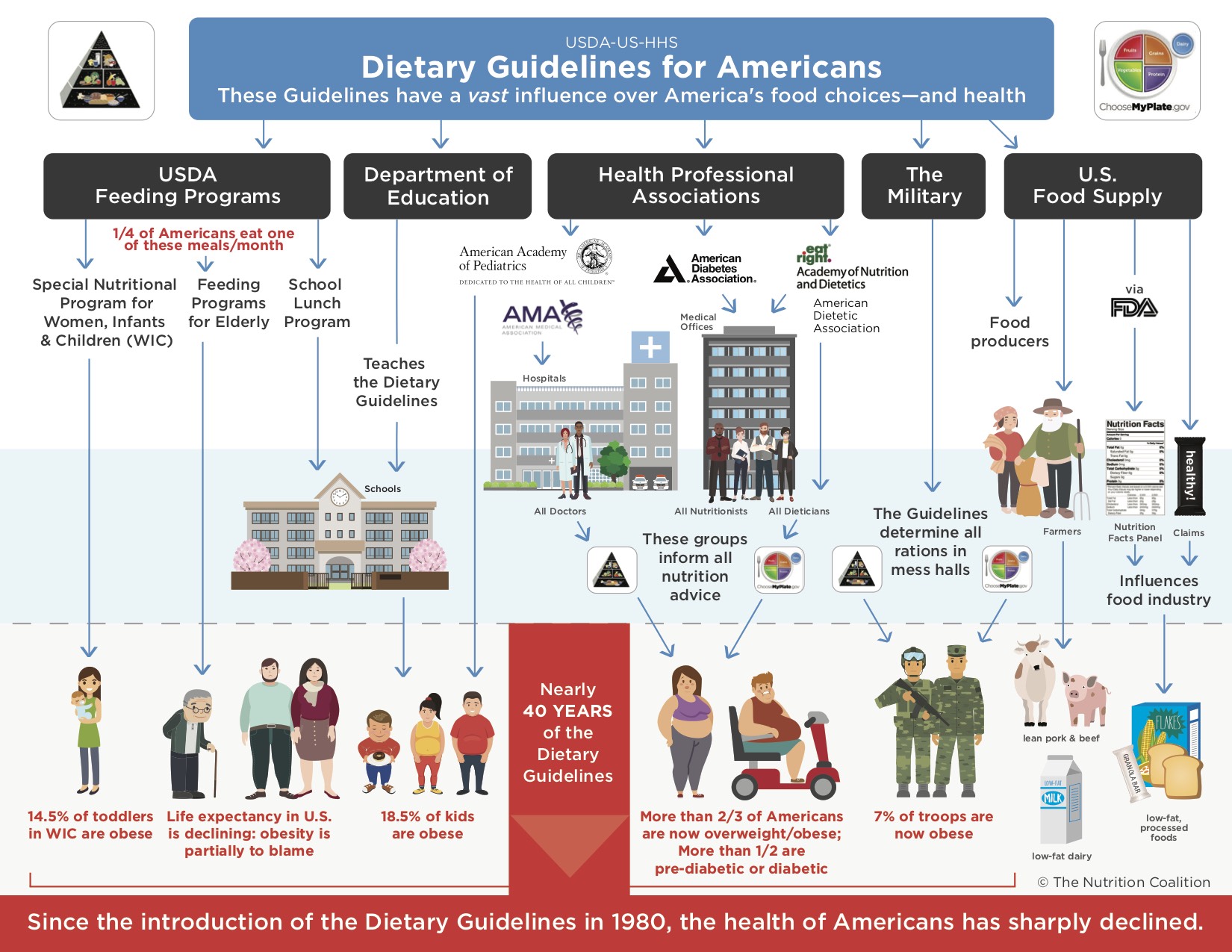
Public Health Outcomes Under the Current Dietary Guidelines
Since the implementation of the dietary guidelines, public health in the United States has deteriorated:
Over 42% of U.S. adults are classified as obese (CDC, 2023)
Approximately 88 million adults have prediabetes, with over 37 million diagnosed with type 2 diabetes
Heart disease remains the leading cause of death
Rates of infertility, mental health disorders, and autoimmune disease are escalating
These alarming trends suggest that current dietary policy is not only ineffective but may be actively contributing to the very conditions it aims to prevent.
Rising Childhood Metabolic Disorders Reflect a Broken System
The nutritional recommendations followed by school systems, pediatricians, and public food programs are grounded in the Dietary Guidelines. Consequently, children are being raised on meals composed of:
Low-fat flavored milks sweetened with sugar
Ultra-processed breakfast cereals marketed as “whole grain”
Lunch trays filled with seed oil-fried meats and fortified starches
The result? A generation plagued by early-onset metabolic syndrome, attention disorders, and compromised immune health. Pediatric fatty liver disease and insulin resistance are no longer rare anomalies; they are the new normal.
Misrepresentation of Nutrient-Dense Animal Foods
Despite their exceptional nutrient profiles and proven benefits, animal-based foods like red meat and full-fat dairy continue to be misrepresented and marginalized in national dietary advice. This section explores how and why these foods are unfairly demonized, and what modern science actually reveals about their role in a healthy human diet.
Red Meat and the Saturated Fat Myth
Despite being one of the most nutrient-dense foods available, red meat continues to be scapegoated in the guidelines. This demonization stems from outdated studies that confound red meat consumption with unhealthy lifestyle habits (e.g., smoking, sedentary behavior, low fruit and vegetable intake).
Grass-fed red meat is an exceptional source of:
Bioavailable iron, zinc, and selenium
B vitamins, including B12
Creatine and carnosine (supporting muscle and brain health)
Instead of celebrating red meat for its nutritional density, the guidelines elevate synthetic meat alternatives composed of isolated soy proteins, genetically modified oils, and chemical additives.
Full-Fat Dairy and the Absurdity of Low-Fat Recommendations
Despite research demonstrating the superior health outcomes associated with whole-fat dairy consumption, the current dietary guidelines recommend low-fat or fat-free dairy products. Numerous cohort studies have found that full-fat dairy is associated with:
Lower risk of obesity
Improved glucose metabolism
Higher levels of HDL cholesterol
Better satiety and reduced overeating
Removing the natural fat from dairy distorts its nutritional integrity and often necessitates the addition of sugar or stabilizers to maintain palatability. This contradicts the goal of reducing added sugars and improving metabolic health.
The Role of Dietary Guidelines in the Proliferation of Ultra-Processed Foods
Far from promoting whole-food nutrition, the U.S. Dietary Guidelines have unintentionally legitimized the rise of ultra-processed food consumption. This section explores how institutional adherence to these recommendations reinforces a nationwide dependence on nutrient-poor, industrialized food products.
Public Programs and Institutional Menus Amplify the Problem
The influence of the U.S. Dietary Guidelines extends far beyond personal food choices. These guidelines shape:
National school lunch programs
Military rations
Hospital patient meals
SNAP (food assistance) benefits
These institutions are often mandated to follow the USDA guidelines, resulting in widespread consumption of:
Enriched white grains
Soy and vegetable oil-laden packaged foods
Fortified, sugar-rich cereals
This systemic reliance on ultra-processed, low-nutrient-density foods has created a national feedback loop of poor health, pharmaceutical dependence, and escalating medical costs.
Recommendations for Evidence-Based Nutritional Reform
As chronic disease rates rise despite decades of following official dietary advice, it is imperative to explore alternative, evidence-based strategies for improving public health. This section outlines practical nutrition reforms rooted in ancestral wisdom and scientific integrity.
Embracing Ancestral Nutrition Principles for Modern Health
A growing body of literature and clinical experience supports a return to ancestral dietary patterns that emphasize whole, unprocessed foods and animal-based nutrition. Key tenets include:
Prioritizing pasture-raised animal proteins and fats
Consuming seasonal produce and fermented foods
Avoiding refined sugars, grains, and seed oils
Supporting metabolic flexibility through intermittent fasting
These principles align with the diets that sustained healthy human populations for thousands of years prior to industrial agriculture.
Policy-Level Changes to Support Nutritional Integrity
To create meaningful change, the following reforms are essential:
Separate the USDA’s roles in agriculture promotion and public health policy
Establish stricter conflict-of-interest rules for DGAC members
Prioritize randomized controlled trials and mechanistic studies over weak observational data
Include regenerative and sustainable food systems as part of national dietary recommendations
Conclusion: Reclaiming Health Through Food Freedom
The current U.S. Dietary Guidelines are built on a crumbling foundation of outdated science, corporate influence, and political compromise. Their perpetuation of high-carbohydrate, low-fat, ultra-processed eating patterns is contributing to a nationwide health crisis that affects individuals from childhood through old age.
But change is possible. Individuals can reclaim their health and challenge a system that profits from chronic illness by prioritizing whole foods, ancestral wisdom, and independent science. Nutritional freedom is not a fringe ideology — it’s a necessary evolution.
The USDA might take decades to admit its mistakes, but your next meal doesn’t have to wait. Choose real food. Trust your biology. And question everything that comes wrapped in shiny packaging with a health claim.