When we look at the health crisis surrounding metabolic dysfunction today, one thing is crystal clear: mainstream medical advice has failed us. We’ve got more people than ever before suffering from type 2 diabetes, obesity, and other metabolic disorders. How could this happen in an era of such medical advancement? Shouldn’t we be conquering these problems by now?
The ugly truth is that mainstream medical advice, specifically when it comes to metabolic health and insulin sensitivity, is not just outdated—it’s dangerously misleading. Instead of focusing on lifestyle changes that address the root cause of metabolic dysfunction, doctors have been prescribing quick-fix solutions that simply mask symptoms, leaving the underlying problem to fester. The result? We’ve created a nation—and increasingly, a world—of diabetics.
And the biggest irony? This isn’t just about diabetes. Metabolic health is critical for everyone. Your ability to regulate blood sugar and maintain insulin sensitivity affects every aspect of your well-being, from energy levels to longevity. Yet, the advice you’ve probably received—cut the red meat and take your meds—has likely done more harm than good.
Glucose Regulation: The Real Foundation of Metabolic Health
Here’s a fact that most people don’t fully understand: glucose regulation is central to your body’s ability to function properly. Glucose, or blood sugar, is the body’s primary fuel source. It’s what powers your brain, muscles, and organs. Without the ability to effectively regulate glucose, everything starts to go haywire.
The system works like this: when you eat carbohydrates, they’re broken down into glucose, which enters the bloodstream. Insulin is then secreted by the pancreas to help transport glucose from the bloodstream into your cells. Once inside the cells, glucose can either be used for energy or stored as glycogen in muscles and the liver for later use.
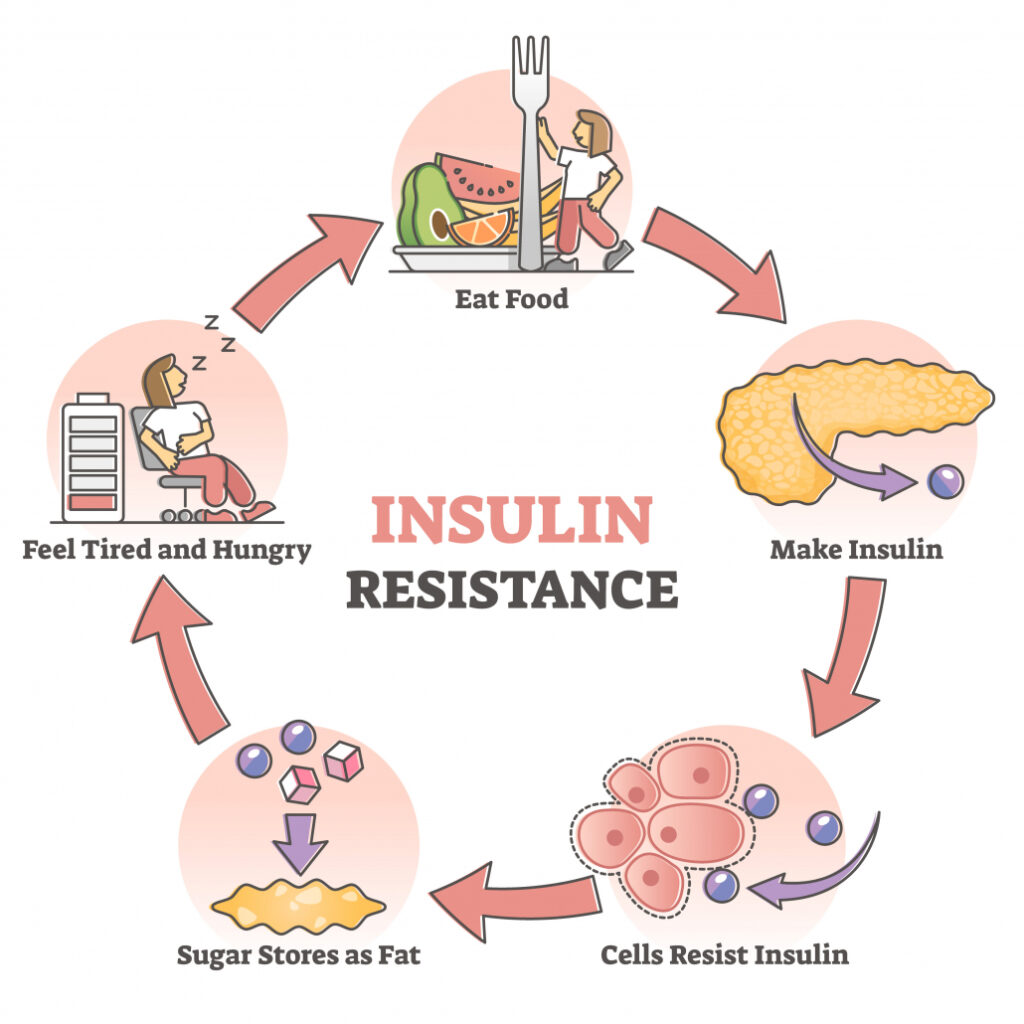
This process is supposed to run like a well-oiled machine. But for many people, it doesn’t. Insulin resistance—where the body’s cells become less responsive to insulin—throws a wrench into the system. As insulin becomes less effective, the body needs to pump out more of it to manage blood sugar levels. Eventually, this leads to chronically elevated blood sugar, or hyperglycemia, and type 2 diabetes.
But here’s what you might not know: the difference between someone who is metabolically healthy and someone with raging type 2 diabetes is only about one teaspoon of extra blood sugar. That’s right—just an extra 5 grams of glucose circulating in the bloodstream is enough to tip the scale from health to disease. This shows how delicate glucose regulation is and how critical it is that we maintain tight control over our blood sugar.
Mainstream Medicine’s Quick Fix: Insulin Medication and Its Flaws
When someone is diagnosed with type 2 diabetes, what’s the typical treatment? Insulin medication, metformin, and perhaps some vague advice about “diet and exercise.” This approach, while it may stabilize blood sugar levels in the short term, does nothing to fix the underlying problem: insulin resistance.
Instead of addressing the root cause, insulin medication simply pushes more glucose into the cells, artificially lowering blood sugar while the real issue continues to worsen. Over time, this leads to a vicious cycle where the body becomes even more insulin resistant, requiring higher doses of medication to achieve the same effect. Not to mention the side effects: weight gain, cardiovascular problems, and a higher risk of other metabolic diseases.
Studies have proven that long-term use of insulin therapy in type 2 diabetics is associated with a higher incidence of cardiovascular disease and weight gain—two outcomes that are the very things we should be preventing in diabetics!
So what should doctors be focusing on instead of prescribing insulin? Improving insulin sensitivity. The key to reversing metabolic dysfunction isn’t flooding the body with more insulin; it’s training the body to use insulin more effectively by addressing the factors that cause insulin resistance in the first place—namely, poor diet, sedentary lifestyle, and lack of muscle mass.
Desensitization: The Insulin Sensitivity and Volume Analogy
Think about this: if you listen to music at 80% volume in your headphones all day long, after a while, that music won’t seem as loud anymore—it might even start to feel like 20%. Your ears adapt and become less sensitive to the constant barrage of sound. This exact concept applies to how our bodies react to excess sugar and carbohydrates.
When you continually eat high amounts of sugar and refined carbohydrates, your body, just like your ears, becomes desensitized. Normally, when you consume carbohydrates, your pancreas releases insulin to help shuttle glucose into your cells for energy. But when you flood your system with sugar—particularly refined and artificial sugars—your body becomes overwhelmed. Insulin levels remain chronically elevated, and eventually, your cells stop responding to insulin as efficiently as they once did. This is insulin resistance, the body’s equivalent to your ears adjusting to high-volume music.
At this point, your body needs to produce more and more insulin just to manage the same amount of glucose, leading to a vicious cycle that puts enormous stress on your pancreas and sets you on the path toward type 2 diabetes. Just like turning up the music to compensate for your reduced hearing sensitivity, your body keeps pumping out more insulin to deal with the same amount of sugar. And, just as with your hearing, this desensitization has long-term consequences.
The fix? Just like giving your ears a break from constant loud noise, your body needs a break from excessive sugar. This doesn’t mean cutting all carbs or sugar, but rather redefining your relationship with carbohydrates and focusing on the right kinds of sugar.
Natural vs. Artificial Sugars: Not All Sugar Is Created Equal
Here’s where things get interesting: not all sugars affect your body the same way. Natural sugars found in whole fruits are very different from the artificial sugars and refined carbohydrates that are abundant in processed foods. Yet, for years, mainstream health advice lumped all sugar together under one umbrella, leading to confusion and unhealthy eating habits.
Let’s break it down:
Artificial and Refined Sugars: These are the sugars found in things like sodas, candy, baked goods, and many packaged snacks. They are highly processed, stripped of any beneficial nutrients, and absorbed quickly into the bloodstream. This rapid absorption leads to a quick spike in blood sugar, which then triggers a large release of insulin. Over time, this can contribute to insulin resistance and metabolic dysfunction. Examples of these sugars include high-fructose corn syrup, cane sugar, and glucose syrup.
Natural Sugars in Fruits: On the other hand, the sugars found in whole fruits—like fructose—come packaged with fiber, vitamins, minerals, and antioxidants. This fiber slows down the digestion and absorption of sugar, preventing rapid blood sugar spikes. Additionally, the nutrients in fruit provide your body with what it needs to properly metabolize the sugars and support overall health. While you’re still consuming sugar, the way it’s processed by the body is vastly different compared to artificial sugars.
For example, eating an apple doesn’t send your blood sugar soaring the way drinking a sugary soda would. That’s because the fiber in the apple slows down the digestion of the sugar, giving your body more time to handle it effectively. Plus, the vitamins and antioxidants in the fruit support your body’s metabolic processes, helping to improve insulin sensitivity.
So, what does this mean for your metabolic health? It’s simple: focus on natural, whole foods. If you’re craving something sweet, opt for fruit rather than candy or pastries. You’ll still get the sweetness your taste buds are looking for, but without the damaging blood sugar spikes and insulin overdrive that come from artificial sugars.
The Role of Muscle in Glucose Regulation
This brings us to the most overlooked aspect of metabolic health: muscle mass. When you think of muscle, you might think of it as something that only athletes or bodybuilders care about. But in reality, muscle is the body’s most important organ for glucose regulation.
Muscle tissue is where the majority of glucose is disposed of after a meal. When you eat carbohydrates, insulin helps shuttle glucose into your muscle cells, where it’s either used for energy or stored as glycogen. The more muscle you have, the more glucose your body can take up and use efficiently.
But here’s the kicker: if you’re not actively working to maintain or build muscle, your ability to regulate glucose is severely compromised. Muscle is your best defense against insulin resistance, but mainstream health advice barely mentions it. Instead, we’ve been told to focus on cardio, low-fat diets, and calorie restriction—all of which do little to improve insulin sensitivity in the long run.
Research has shown the role of muscle mass in improving insulin sensitivity, showing that individuals with higher muscle mass have better glucose regulation and a lower risk of developing insulin resistance and type 2 diabetes. Strength training, in particular, has been shown to increase insulin sensitivity and improve glucose disposal, making it one of the most powerful tools for preventing and reversing metabolic dysfunction.
So why isn’t this the first thing your doctor tells you when you’re diagnosed with type 2 diabetes? Because mainstream medicine is more focused on managing symptoms than addressing the root cause. And that’s exactly why we’re in the midst of a diabetes epidemic.
Insulin Sensitivity: The Key to Longevity and Health for Everyone
Now, you might be thinking, “I don’t have diabetes, so why should I care about insulin sensitivity?” The answer is simple: insulin sensitivity is crucial for everyone, not just diabetics.
Even if you’re not currently struggling with elevated blood sugar or insulin resistance, maintaining good insulin sensitivity is essential for preventing metabolic diseases, maintaining a healthy weight, and optimizing energy levels. Poor insulin sensitivity is linked not only to type 2 diabetes but also to obesity, heart disease, and even Alzheimer’s disease—often referred to as “type 3 diabetes” due to its connection with insulin resistance.
A healthy, insulin-sensitive body is better at managing blood sugar, burning fat, and maintaining energy balance. So whether your goal is to prevent disease, improve athletic performance, or simply feel better, insulin sensitivity should be at the top of your priority list.
How Our Modern Lifestyle Wrecks Insulin Sensitivity
So, what’s causing the widespread insulin resistance we see today? A lot of it comes down to our modern lifestyle. Let’s break down the major culprits:
1. Processed Foods and Refined Carbohydrates
We’ve been bombarded with highly processed foods that are packed with refined carbohydrates and sugars. These foods spike blood sugar levels, causing the pancreas to pump out large amounts of insulin. Over time, this constant barrage of insulin leads to insulin resistance, where the cells become desensitized to insulin’s effects.
Research proves that diets high in refined carbohydrates and processed foods are strongly linked to the development of insulin resistance and type 2 diabetes. The researchers emphasized the importance of replacing these foods with whole, unprocessed foods to improve insulin sensitivity.
2. Sedentary Behavior
In today’s world, we sit more than ever before. Whether it’s at a desk, in front of a screen, or during long commutes, our modern lifestyle promotes inactivity. The problem? Sedentary behavior is one of the fastest ways to lose insulin sensitivity.
When you’re not moving, your muscles aren’t using glucose. And when your muscles aren’t using glucose, insulin levels remain elevated. Over time, this leads to insulin resistance. A study by the American Diabetes Association found that just a few days of inactivity can significantly reduce insulin sensitivity, highlighting the importance of regular movement for maintaining metabolic health.
3. Poor Sleep and Circadian Disruption
It’s not just diet and exercise that matter—sleep plays a crucial role in metabolic health. Poor sleep, especially chronic sleep deprivation, wreaks havoc on insulin sensitivity. Even a single night of bad sleep can reduce insulin sensitivity by as much as 30%.
And it’s not just sleep quality that matters. Blue light exposure from screens and artificial lighting is a major disruptor of our circadian rhythms, which in turn affects our insulin sensitivity. As I’ve written in my article, Impact of Artificial Light on Global Obesity and Wellness, blue light exposure, especially at night, disrupts melatonin production, throwing off our sleep patterns and metabolic processes. This disruption is linked to insulin resistance, weight gain, and increased risk of type 2 diabetes.
4. Stress and Cortisol
Chronic stress is another major player in the insulin resistance game. When you’re stressed, your body releases the hormone cortisol, which raises blood sugar levels and makes your cells more resistant to insulin. Over time, chronic stress can lead to elevated blood sugar, weight gain, and insulin resistance.
Practical Tools to Improve Insulin Sensitivity and Metabolic Health
So, how can you reverse insulin resistance and improve your metabolic health? Here are some powerful, science-backed strategies:
1. Build Muscle Through Resistance Training
We’ve already established that muscle is the key to glucose regulation. Start incorporating resistance training into your weekly routine—aim for at least 3-4 sessions per week. Focus on compound movements like squats, deadlifts, and presses to build overall muscle mass and improve insulin sensitivity.
2. Fix Your Diet
Ditch the refined carbs and processed foods that spike your blood sugar. Focus on whole, unprocessed foods rich in protein, healthy fats, and naturally occurring carbohydrates. Protein and fat help slow down the absorption of glucose, keeping your blood sugar levels stable.
3. Incorporate Cold Exposure
Cold exposure, through ice baths or cold showers, has been shown to increase insulin sensitivity. Cold activates brown fat, which burns glucose for energy, improving glucose disposal and lowering blood sugar.
4. Blue Light Blocking Glasses
Since blue light disrupts sleep and metabolic health, wearing blue light-blocking glasses in the evening can help protect your circadian rhythms and improve insulin sensitivity. Brands like Ra Optics offer glasses designed to block harmful blue wavelengths and help regulate your body’s natural rhythms.
5. Walk After Meals
Walking after meals helps muscles take up glucose, preventing blood sugar spikes. Aim for a 10-15 minute walk after each meal to improve insulin sensitivity and overall metabolic health.
6. Prioritize Sleep
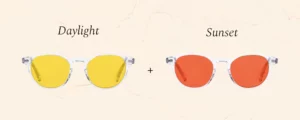
Get at least 7-8 hours of quality sleep each night. Develop a nighttime routine that limits exposure to artificial light, and use blue light-blocking glasses if needed. Poor sleep equals poor metabolic health, so prioritize your rest.
Creating a sleep-friendly environment is key. Dim the lights in the evening, avoid screens at least an hour before bed, and keep your room cool and dark. Consistent, high-quality sleep can dramatically improve how your body handles glucose and insulin.
7. Sunlight Exposure
We often overlook the role of natural sunlight in metabolic health, but it’s crucial for maintaining insulin sensitivity and regulating hormones. Sunlight exposure helps stimulate vitamin D production, which plays a key role in insulin function and blood sugar control. Studies have shown that vitamin D deficiency is linked to insulin resistance and an increased risk of type 2 diabetes.
Spending time in the sun—preferably in the morning—can also help regulate your circadian rhythms, which improves sleep quality, reduces stress, and ultimately supports better insulin sensitivity. Aim for at least 15-30 minutes of direct sunlight exposure each day to boost your vitamin D levels and support overall metabolic health.
8. Incorporate Fasting
Intermittent fasting or extended fasting periods can be powerful tools for improving insulin sensitivity. Fasting gives your body a break from constantly processing food and allows your insulin levels to drop, which helps reset insulin sensitivity. Studies show that intermittent fasting can lower insulin levels, reduce blood sugar, and improve metabolic markers.
One of the simplest ways to incorporate fasting is through a daily fasting window, such as the 16/8 method, where you fast for 16 hours and eat within an 8-hour window. This strategy not only reduces the frequency of insulin spikes but also helps your body become more efficient at using stored fat for energy, improving metabolic flexibility.
9. Use a Continuous Glucose Monitor (CGM)
Continuous glucose monitors (CGMs) have become increasingly popular, not just for diabetics but also in health and fitness circles. These wearable devices provide real-time feedback on your blood glucose levels, allowing you to see how different foods, activities, and lifestyle factors affect your blood sugar.
By using a CGM, you can track how your body responds to specific meals, exercise routines, or even stress, giving you the information you need to make better dietary and lifestyle choices. This personalized data is invaluable for anyone looking to improve their insulin sensitivity and overall metabolic health.
The Bottom Line: Fixing the Metabolic Crisis
Mainstream medical advice has been leading us astray for years, pushing drugs and quick fixes instead of addressing the root causes of metabolic dysfunction. The key to reversing this epidemic of type 2 diabetes, obesity, and insulin resistance isn’t more medication—it’s about building muscle, improving insulin sensitivity, and making simple yet powerful lifestyle changes.
Your metabolic health isn’t just important if you have diabetes—it’s the foundation of longevity and vitality for everyone. So don’t wait for a diagnosis to start taking control of your health. By following the strategies outlined here, you can become a metabolic powerhouse and avoid the chronic diseases that are plaguing our modern world.