In the modern world, we’re surrounded by things we can’t see. Invisible toxins in the air, on our clothes, in our food, and even leaching out of our phones. For a growing number of people, these everyday exposures are doing something far more sinister than causing a little irritation. They’re rewiring the body’s tolerance system. Enter Toxicant-Induced Loss of Tolerance—or TILT. It’s not a trendy acronym. It’s a quietly growing health crisis.
What is Toxicant-Induced Loss of Tolerance (TILT)?
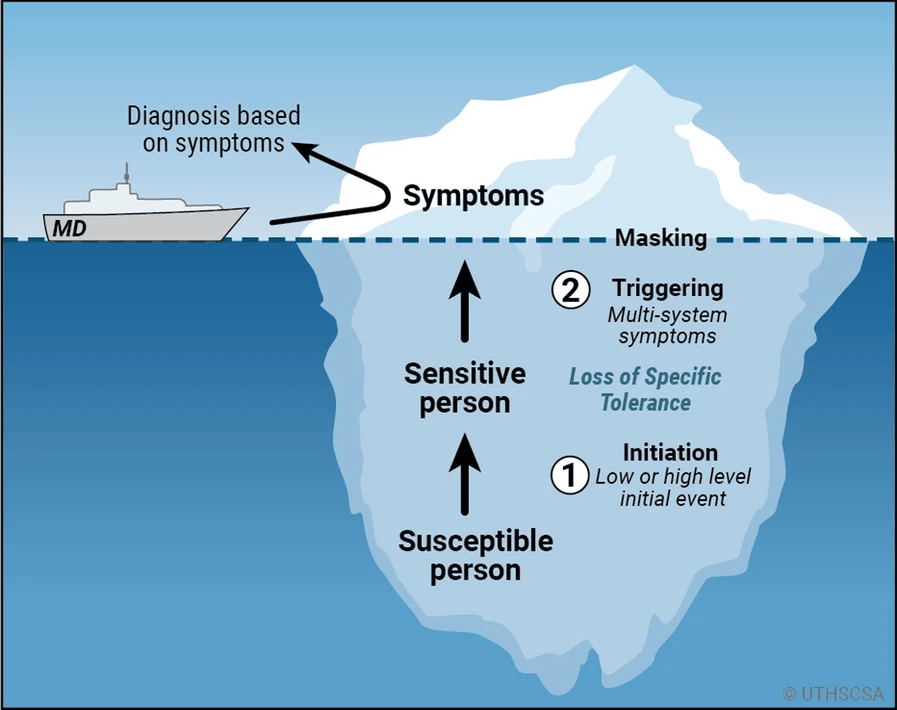
TILT is a two-step disease process. First, there’s the initiation—a major exposure or repeated low-level exposures that damage the nervous or immune system’s ability to regulate responses to environmental inputs. Then comes the triggering phase. After initiation, people suddenly find themselves reacting to chemicals, foods, medications, or even smells that never used to bother them. These aren’t allergic reactions in the conventional sense—there’s no IgE involvement—but the symptoms are real, multisystemic, and life-altering.
People with TILT can develop headaches, brain fog, chronic fatigue, rashes, breathing issues, and a host of vague but debilitating symptoms. Often, these symptoms appear with no clear pattern or cause, leaving patients gaslit by doctors and bewildered by their own bodies.
The Triggers: Just the Tip of the Iceberg
This is the part that confuses most people, where symptoms seem to come out of nowhere. However, they’re not random. They’re the result of a body that has already been overwhelmed.
Once initiation has occurred, the body’s filter is damaged. The immune system and nervous system no longer respond normally to everyday substances. What used to be harmless—a spritz of cologne, a drive past a gas station, the scent of dryer sheets from a neighbor’s house—can now provoke a storm of symptoms.
Common triggers include:
Fragrances (perfume, cologne, air fresheners)
Gasoline fumes and car exhaust
Cleaning products and synthetic detergents
Off-gassing from furniture or carpets
Cigarette smoke and vape aerosols
Pesticide and herbicide drift
Mold and mildew odors
Certain foods and additives (especially after chemical exposure)
And the number of triggers can multiply over time. Some people report developing dozens—sometimes hundreds—of specific intolerances after their body “tilts.”
What’s visible to the doctor (or anyone else) is just the tip of the iceberg. Beneath the surface is a tangled web of physiological damage and unrecognized environmental inputs.
Not Just Anecdotes: The 2021 Study That Changed Everything
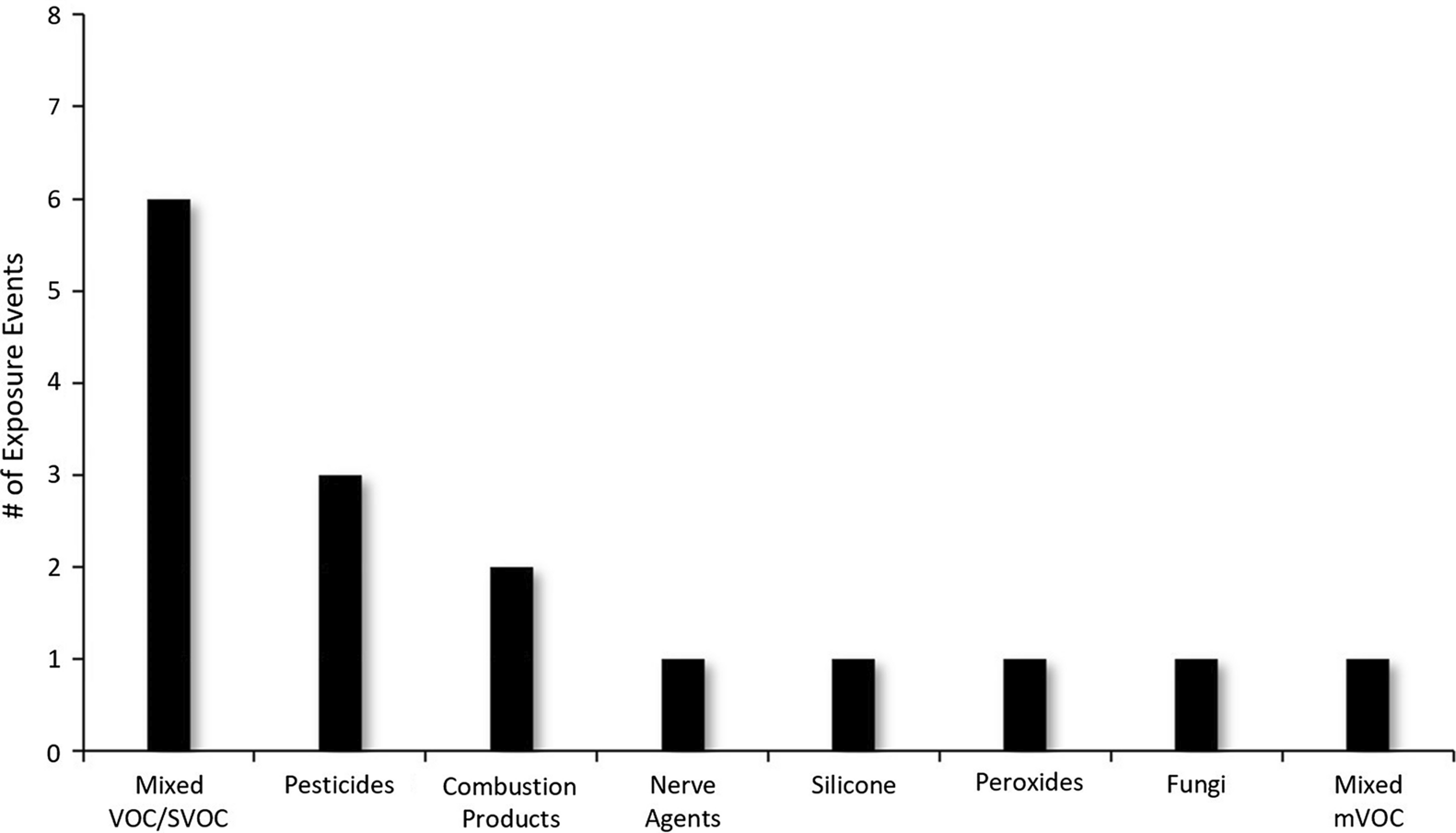
A massive 2021 study published in Environmental Sciences Europe pulled back the curtain on this phenomenon. Researchers reviewed eight high-profile chemical exposure events linked to widespread illness and chemical intolerance:
EPA Building Renovation (carpet chemicals, VOCs)
Gulf War Veterans (nerve agents, pesticides)
Casino Workers (pesticide exposure)
Aircraft Cabin Fume Events (jet oil additives)
9/11 First Responders (building combustion chemicals)
Surgical Implants (leaching silicone and metals)
Mold-Infested Homes (VOC-emitting fungi)
Tunnel Workers (gasoline vapor exposure)
Each case revealed a troubling pattern. People exposed to specific chemical groups—mainly VOCs, SVOCs, pesticides, and combustion byproducts—began reporting new sensitivities and multi-system symptoms. This wasn’t a one-off. It was consistent across different events, countries, and demographics.
The Chemicals That Keep Showing Up
Let’s name names. These aren’t just obscure lab compounds—many of them are hiding in plain sight, woven into the fabric of daily life. And they’re some of the most common repeat offenders seen in TILT initiation events.
Xylene, benzene, acetone – found in paint thinners, nail polish remover, and gasoline fumes
Organophosphates and carbamates – widely used in insecticides, lawn sprays, and pest control
Phthalates and flame retardants – hidden in electronics, upholstery, and children’s toys
Formaldehyde – used in pressed-wood products, glues, and wrinkle-free fabrics
Whether people were exposed to one or to a cocktail of these substances, the results were often life-altering—sometimes devastating. These chemicals show up time and again in studies, case reports, and patient histories. The pattern is hard to ignore.
The sobering reality? You don’t need to work in a factory or live near a chemical plant to be exposed. Everyday environments—homes, offices, schools—can be saturated with these compounds, especially when ventilation is poor or new materials are introduced.
The Sick Building That Made the EPA Sick
Yes, the Environmental Protection Agency was at the center of one of the earliest known TILT outbreaks. In 1987, 27,000 square yards of new carpet were installed at EPA headquarters. Employees quickly reported symptoms, some so severe they required hospitalization. The culprit? 4-phenylcyclohexene (4-PCH), a byproduct of synthetic carpet adhesives. Even more unsettling: It wasn’t just the 4-PCH. The carpet was off-gassing a stew of other VOCs.
Here’s what made this case so notable:
The event involved EPA scientists and experts—people trained in toxicology and environmental health
Exposure happened during a routine renovation, not an industrial accident
Symptoms included headaches, rashes, dizziness, and fatigue, often worsening each day workers returned to the building
Dozens of workers quit their jobs due to ongoing illness
And that’s the thing about TILT—it’s rarely one chemical doing all the damage. It’s the combination. The cumulative burden. It’s the body’s loss of tolerance to a symphony of synthetic inputs that never should have shared the same air.
Gulf War Illness: A Case Study in TILT
When hundreds of thousands of Gulf War veterans came home reporting a baffling array of health issues—fatigue, brain fog, joint pain, gastrointestinal distress—it wasn’t long before researchers began to notice a pattern. These weren’t just random post-combat stress symptoms. They pointed to something deeper, something environmental, and all too familiar: TILT.
Veterans were exposed to a unique and disturbing cocktail of chemicals, including:
Nerve agents such as sarin and cyclosarin
Organophosphate pesticides used for pest control in tents and on uniforms
Pyridostigmine bromide pills (PB) meant as a defense against nerve gas, but disruptive to acetylcholinesterase
Burn pits filled with plastics, medical waste, and jet fuel
Oil well fires, which blanketed the region in combustion byproducts
Why These Exposures Matter
Each of these chemicals affects the cholinergic nervous system, particularly the enzyme acetylcholinesterase, which regulates communication between nerves and muscles. When disrupted, this system can lead to widespread neurological dysfunction.
Veterans weren’t imagining it. The VA itself acknowledges that about 30% of Gulf War veterans meet the case definition for Gulf War Illness, a condition that overlaps heavily with the symptoms and mechanisms of TILT.
Mold: The Biological Chemical Factory
Mold is far more than a common allergen. It’s a biological chemical factory, capable of producing volatile organic compounds (VOCs), mycotoxins, and spores that have profound effects on the nervous system, immune function, and even psychological health. These aren’t just seasonal sniffles or musty odors—they’re complex exposures that can initiate or exacerbate TILT.
In one Finnish study of over 1,000 mold-exposed patients, about 50% developed full-blown TILT over time. That’s not a fringe case—that’s an epidemic hiding in water damage.
Why Mold Matters in TILT
Mold VOCs have been shown to produce neurological damage in animal studies, including Parkinson’s-like symptoms.
Damp buildings also release formaldehyde and degraded resin byproducts that act synergistically with mold toxins.
Moldy homes often contain bacteria, dust mites, and degraded building materials, compounding the toxic load.
Signs of Mold-Induced TILT:
Sensitivities to multiple smells, foods, or medications
Cognitive decline and memory fog
New onset of chemical intolerance following water damage
This is why simply cleaning the visible mold isn’t enough. It’s not just what you see—it’s what you breathe. Mold can silently restructure your tolerance blueprint, making you reactive not just to mold, but to everything else.
TILT Isn’t Just Rare—It’s Underdiagnosed
Up to 36% of Americans report some form of chemical intolerance. Around 5–12% report a doctor-diagnosed condition such as “multiple chemical sensitivity” (MCS). Despite this, the medical establishment remains largely unaware—or worse, dismissive.
Patients are often referred to psychiatrists, told their symptoms are “in their head”, or bounced around between specialists based on surface-level symptoms. Neurologist, pulmonologist, gastroenterologist… no one connects the dots because the model for TILT isn’t taught in med school.
A Disease Without a Home in Medicine
Why isn’t TILT officially recognized? Simple: it doesn’t fit neatly in a box. It’s not a classic allergy. There’s no IgE involvement. Skin prick tests? Useless. Bloodwork? Often normal.
The problem is how medicine is structured. Are you present with shortness of breath? You see a pulmonologist. Digestive issues? Gastroenterologist. Brain fog? Psychiatrist. But TILT doesn’t play by those rules. It’s multi-systemic and rooted in environmental triggers that most doctors never test for.
And the longer it’s dismissed, the worse it gets. Triggers stack. People become housebound, unable to tolerate everyday products. Some live in trailers in the woods. Others isolate themselves from society just to avoid perfume or cleaning products.
Prevention Is the Only Cure (For Now)

There’s no pharmaceutical for TILT. No miracle shot. But there are tools:
Avoid initiating exposures—remodeling projects, pesticides, new carpets, or environments with known chemical pollutants
Eliminate triggers—fragrances, solvents, plastics, synthetic detergents
Use air purification—HEPA filters, activated charcoal, and ideally ventilation from outside air
Minimize tech EMFs, such as wireless radiation emitted from AirPods, smartwatches, and cell phones, which many TILT sufferers also become sensitive to
Grounding and outdoor time to reset the body’s stress and immune responses
The QEESI and BREESI: Tools That Actually Help
While there’s no silver bullet for TILT, having the right screening tools can make all the difference, both for individuals and healthcare providers trying to navigate this complex condition.
The QEESI (Quick Environmental Exposure and Sensitivity Inventory) is a comprehensive tool that helps assess a person’s level of intolerance across multiple domains:
Chemical intolerance
Food intolerance
Symptom severity
Life impact
Masking index (for identifying hidden exposures)
This validated questionnaire uses a 0–100 scoring system and is used internationally in both research and clinical settings.
The BREESI (Brief Environmental Exposure and Sensitivity Inventory) is a simplified screener made up of just 3 quick questions. It’s especially useful in primary care or occupational health settings where time is limited.
Here’s what sets these tools apart:
They help identify TILT when traditional lab tests come up empty
They empower patients to track symptoms and identify patterns
They’re validated in peer-reviewed research and accepted globally
These aren’t pseudoscientific checklists—they’re used by researchers at institutions like MIT, the University of Texas, and even health agencies across Europe.
For people who’ve been dismissed or told “it’s all in your head,” these tools offer something rare: validation, clarity, and a path forward.
Final Thoughts: How Many More Will Tilt Before We Wake Up?
This isn’t fringe. This isn’t “anxiety.” This is a growing public health crisis, fueled by synthetic chemical production that’s exploded since WWII. From less than 1 billion pounds of synthetic organics per year pre-war to over 460 billion pounds by the mid-90s, we’ve marinated modern life in petrochemicals.
It’s no wonder the body is fighting back.
TILT is what happens when modern chemistry collides with ancient biology. We weren’t built for this world of off-gassing furniture, pesticide-laden food, and synthetic fragrances in every public space. And yet, here we are. Sick, sensitive, and searching for answers.
If there’s one takeaway from all this, it’s that TILT isn’t rare. It’s just rarely recognized.
The sooner public health and medical institutions begin addressing TILT as a legitimate, two-phase disease process, the better we can serve the millions suffering in silence.