Ozempic and other GLP-1 agonists have been hailed as revolutionary weight-loss drugs, offering dramatic results without major lifestyle changes. But beneath their appeal lies a deeper issue—the long-term risks of hijacking the body’s natural metabolic systems.
While these drugs suppress appetite and may provide cardiovascular benefits, they also come with serious side effects like muscle loss, gastroparesis, and gallbladder disease. Worse, once users stop taking them, weight regain is almost inevitable, often accompanied by metabolic damage that makes future weight loss even harder.
This article explores the hidden dangers of Ozempic, questioning whether short-term weight loss is worth the long-term consequences. Are we truly improving health, or just creating a new cycle of pharmaceutical dependency?
The Seduction of Quick Fixes: Why Ozempic is So Popular
Ozempic and other semaglutides work by mimicking the hormone GLP-1, which plays a role in regulating appetite and insulin levels. By slowing digestion and suppressing hunger, these drugs make it easier to eat less and lose weight. And for millions struggling with obesity, this seems like a miracle solution—no dieting, no exercise, just a weekly injection.
But here’s the problem: the ease of pharmaceutical intervention distracts from the fundamental causes of weight gain—ultra-processed foods, sedentary lifestyles, and metabolic dysfunction. Instead of addressing these root issues, Ozempic offers a chemical shortcut that keeps people dependent on a drug rather than empowering them to regain control of their health.
Moreover, stopping the medication often leads to rapid weight regain, trapping users in a cycle of dependency. That’s not a cure—it’s a business model.
Another issue is the misleading marketing surrounding these drugs. While initial studies and testimonials make Ozempic seem like a magic bullet, the long-term consequences are rarely emphasized. Many users experience weight regain, new health issues, or severe side effects that were never fully disclosed when they first started treatment.
The Hidden Dangers of Ozempic and Semaglutides
1. Sudden Blindness and Vision Damage
Recent studies suggest that semaglutide users may be up to 7.64 times more likely to develop a rare eye condition called non-arteritic anterior ischemic optic neuropathy (NAION), which can lead to permanent blindness. Even more alarming, Ozempic has been linked to worsening diabetic retinopathy, particularly in those with poorly managed blood sugar levels.
Vision issues may be a result of drastic metabolic changes that are unnatural and poorly understood. The forced reduction of insulin resistance can cause unintended effects, making this treatment more of a gamble than a reliable solution.
2. Loss of Muscle and Metabolism Dysfunction
Weight loss from Ozempic is not necessarily fat loss. Many users are losing muscle mass, connective tissue, and even bone density. Worse, prolonged use of semaglutides can lower resting metabolic rates, making it harder to maintain weight loss once off the drug. This means that over time, users may end up in a worse metabolic state than when they started.
Sarcopenia, or muscle loss, is an often-overlooked consequence of rapid weight loss via unnatural means. Lean muscle mass is crucial for metabolic function, mobility, and longevity. Without proper resistance training and sufficient protein intake, Ozempic users may experience a net-negative impact on their health.
Additionally, the weight lost with Ozempic is often regained once the drug is discontinued. This is because these drugs do not correct poor dietary habits or lack of exercise—only the symptoms of these underlying issues.
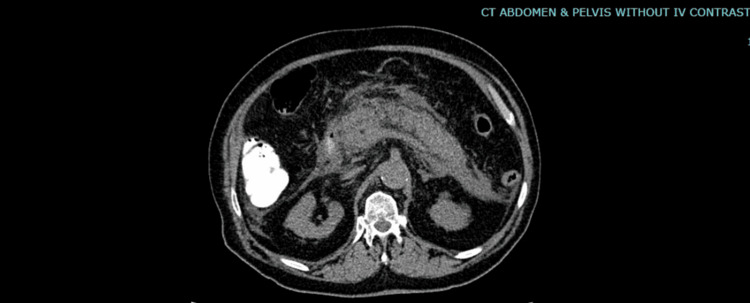
3. Gastrointestinal Issues and Stomach Paralysis
One of the most widely reported side effects of Ozempic is gastroparesis, a condition where the stomach takes too long to empty food. This can lead to nausea, vomiting, bloating, and severe discomfort. In some cases, users have developed persistent stomach paralysis, which can be irreversible.
The body’s natural digestive rhythm is thrown off balance by these medications, further proving that pharmaceutical shortcuts do not create sustainable solutions. Instead of achieving metabolic health, users may be setting themselves up for a future riddled with digestive issues.
4. Pancreatitis and Gallbladder Issues
Semaglutides have been linked to inflammation of the pancreas (pancreatitis) and increased risk of gallbladder disease, including gallstones. Some users have even required emergency gallbladder removal after prolonged use of Ozempic.
The gallbladder plays a crucial role in fat digestion. If these weight-loss drugs disrupt bile production and fat metabolism, they create new, long-term health issues that require more medical intervention down the line.
The Psychological Toll of Dependency
Relying on a drug for weight management can create a dangerous psychological dependency. Instead of building the habits necessary for lasting health, users become reliant on an external substance to control their weight. What happens when they stop taking it? For many, weight returns just as quickly as it was lost, leading to frustration, yo-yo dieting, and a deepened reliance on the medical-industrial complex.
Additionally, recent research suggests that semaglutide use may be linked to depressive symptoms. A case report from Peking Union Medical College Hospital documented two patients who developed depression within a month of starting semaglutide. One was a middle-aged man with no history of depression who experienced fatigue, decreased motivation, and difficulty concentrating. The other was a middle-aged woman with recurrent depressive disorder whose symptoms worsened significantly after beginning treatment. In both cases, depression symptoms improved once semaglutide was discontinued.
This suggests that semaglutide may negatively impact brain chemistry, potentially by altering dopamine levels or affecting neural pathways related to mood regulation. While more research is needed, this is a concerning sign that weight loss drugs like Ozempic may come with unintended mental health consequences.
The Pharmacological Overload: At What Cost Are We Hijacking Our Natural Systems?
Dr. Andrew Huberman and Dr. Zachary Knight highlight both the perceived benefits and serious concerns surrounding GLP-1 agonists like Ozempic. On one hand, these drugs curb appetite, regulate blood sugar, and may even reduce cravings for addictive substances. Some research also suggests that they could have anti-inflammatory effects, potentially explaining the cardiovascular benefits observed in clinical trials.
However, the real question is: At what cost are we hijacking our natural systems?
GLP-1 drugs introduce hormone levels up to 10,000 times higher than what the body naturally produces, an unprecedented disruption of metabolic function. While these drugs may provide short-term advantages, they also override essential regulatory pathways in ways we don’t fully understand.
One alarming concern is their impact on dopamine and motivation pathways. By suppressing cravings, these drugs may also blunt reward-driven behavior, leading to reduced drive, emotional instability, and even anhedonia (inability to feel pleasure). This raises serious questions about long-term neurological consequences beyond just weight loss.
Additionally, pharmaceutical companies are pushing further into multi-hormone agonists, combining GLP-1 with other regulators to mimic bariatric surgery in drug form. While this may produce greater weight loss, it moves further away from natural metabolic balance, raising ethical concerns about how far we should go in chemically altering our biology.
Ultimately, while the benefits of GLP-1 drugs may seem promising, the broader question remains: Are we trading long-term health for short-term gains, all in the name of convenience?
The Bigger Picture: The Medical-Industrial Complex and Its Profit Motive

There’s a reason Ozempic and similar drugs are being pushed so aggressively—they’re incredibly profitable. The weight-loss industry, driven by pharmaceuticals, is a multi-billion-dollar market, and companies like Novo Nordisk (the makers of Ozempic) are capitalizing on society’s desperation for quick fixes.
The weight loss drug market is estimated to be worth $100 billion by 2030, with some analysts forecasting $200 billion within the next decade. In 2023 alone, Novo Nordisk and Eli Lilly made billions from GLP-1 drugs, and there are now over 50 new weight loss drugs in clinical development from approximately 40 companies.
Perhaps most concerning is the corporate strategy to expand the use of weight-loss drugs beyond obesity. Big Pharma is actively lobbying for insurance coverage and regulatory approvals to market these drugs for cardiovascular benefits, sleep apnea, and even fatty liver disease—potentially creating an even broader consumer base reliant on lifelong medication.
The unfortunate reality is that most doctors and healthcare providers operate within this system, often pushing pharmaceutical interventions instead of advocating for true lifestyle changes. After all, there’s far more money in a lifelong customer than in a patient who heals themselves through diet and exercise.
The Real Solution: Taking Back Control of Your Health
1. Prioritize Whole, Unprocessed Foods
The biggest driver of obesity is ultra-processed food consumption. Stick to whole, nutrient-dense foods like grass-fed meats, organic fruits, and vegetables, and healthy fats (such as beef tallow), and avoid seed oils and refined sugars.
2. Strength Training and Movement
Instead of losing muscle mass through pharmaceutical interventions, focus on building muscle. Strength training increases metabolic rate, improves insulin sensitivity, and promotes long-term fat loss.
3. Metabolic Flexibility and Fasting
Developing metabolic flexibility—your body’s ability to efficiently switch between burning carbs and fat—leads to natural weight regulation. Practices like intermittent fasting and circadian eating can help reset hunger hormones and improve overall metabolic health.
4. Get Enough Sleep and Reduce Stress
Chronic stress and sleep deprivation wreak havoc on hormones like cortisol, insulin, and ghrelin, which regulate hunger and fat storage. Prioritizing high-quality sleep and stress management is critical for long-term health.
5. Address Nutrient Deficiencies Naturally
Rather than relying on drugs to suppress appetite, address the real deficiencies that drive cravings. Magnesium, B vitamins, omega-3s, and amino acids all play key roles in satiety and energy regulation.
6. Improve Insulin Sensitivity Naturally
Rather than using a drug to force insulin resistance improvements, focus on blood sugar regulation through low-glycemic eating, resistance training, and circadian-based meal timing. These strategies work with the body’s natural biology rather than against it.
The Final Verdict: Reject the Pharmaceutical Shortcut
The rise of Ozempic and other semaglutides is a symptom of a larger societal problem—we’ve been conditioned to believe that health comes from a pill, an injection, or a prescription, rather than from our own habits and choices. The reality is that true health is built from the inside out.
Yes, losing weight can be hard. But the hard way is often the right way. Rather than falling into the trap of medical dependency, take control of your health through proper nutrition, movement, sleep, and stress management. Not only will your results be more sustainable, but you’ll also avoid the long list of side effects and long-term damage that these weight-loss drugs can bring.
Your body was designed to thrive—without pharmaceutical intervention. The choice is yours: do you want temporary results with long-term consequences, or do you want lasting health and vitality? The answer should be obvious.
Ditch the quick fix. Choose real health.